How Medical Billers and Coders Interpret Patient Records
- Medical Billing and Coding
-
 Authored by
Tashonda Shaw
Authored by
Tashonda Shaw
- Updated November 4, 2025
- 1.9k views
Medical billing and coding may be the ideal choice if you’re interested in working in healthcare but prefer a comfortable office environment over a hospital setting. However, the significant question remains—how can one decipher all those complex patient records?
Initially, it might seem somewhat confusing. There are specific codes for everything, whether it’s a sore throat or a major surgery. You must review the records, understand what occurred, and code it appropriately. In this blog, you’ll learn how medical billers and coders read and interpret patient files and the importance of this process.
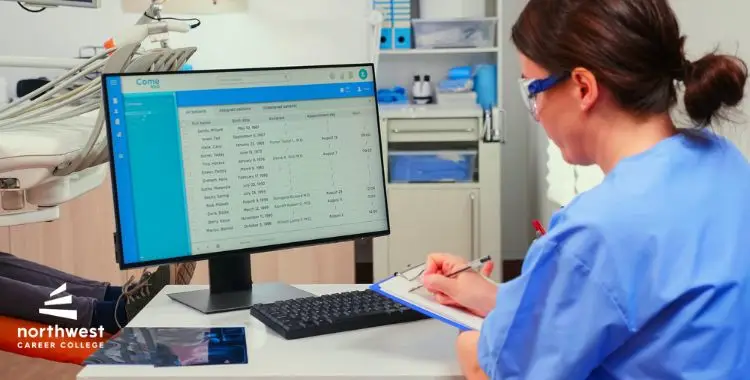
Table of Contents
Familiarizing Medical Codes
Medical billers and coders have a specialized method of coding the events that occurred during a patient visit. These codes inform insurance companies about the type of treatment a patient received and enable them to pay physicians for their services. There are three primary types of codes:
- ICD codes (diagnoses)
- CPT codes (procedures)
- HCPCS codes (supplies and services)
As a medical biller and coder, you will need to understand these codes to read patient records accurately. Proper code reading prevents billing errors, ensures the correct payment to healthcare providers, and facilitates smoother insurance procedures for all parties involved.
Reading Patient Records
Medical billers and coders thoroughly review all information in a patient’s file to accurately code and bill a patient’s record. These include:
- Doctor’s notes
- Lab reports
- Treatment regimens
- Prescribed medications
You will search for the most critical data to guide them in assigning the appropriate codes for the diagnoses and procedures performed.
The job requires tremendous attention to detail. You must double-check that the codes you apply align with the recording in the patient’s file. One missing detail can result in the wrong coding, delayed billing, or even denial of insurance payments. By double-checking the medical records, you ensure that both providers and patients receive fair treatment.
Following Coding Guidelines
Assigning medical codes requires strict guidelines, which are continuously revised to reflect new developments in medical processes and treatment protocols. Coders need to understand how to utilize the guidelines to use the latest and correct codes.
Learning these regulations is a significant step in becoming a successful medical biller and coder. If the incorrect code is used, it can create issues with insurance companies, potentially leading to denied or delayed claims.
Maintaining Privacy and Accuracy
Medical billers and coders must also ensure that the information they deal with is confidential. Patient data includes personal and private health data, and it’s their responsibility to keep it safe. One must adhere to laws such as the Health Insurance Portability and Accountability Act (HIPAA) to keep all patient information safe and secure.
As a medical biller and coder, confidentiality and precision are crucial. You’ll be trusted to handle sensitive material, and it’s up to you to ensure it’s used and stored correctly. That trust is critical to the healthcare system.
Communication with Providers and Insurers
After medical billers and coders have applied the appropriate codes, you will forward the data to insurance companies to receive payment. Occasional errors or the need for supplemental data do occur, though. Medical billers and coders must liaise with healthcare providers and insurance companies to resolve discrepancies or clarify data when this happens.
Clear communication is essential in this portion of the work. If a claim is denied, you must work with the insurance company and the healthcare provider to resolve the problem. Effectively explaining treatment details and codes can streamline the process and eliminate potential issues in the future.
Conclusion
Medical billers and coders play an essential role in ensuring that patients’ medical records are accurately interpreted and that healthcare providers receive payment for their services. You will examine patients’ medical files, assign the correct codes, and communicate with insurance providers. Each of these tasks contributes to the smooth functioning of the healthcare system. Are you ready to begin a fulfilling career in medical billing and coding? Northwest Career College provides a program that will equip you with the skills necessary to thrive in this expanding field. Enroll now!



